What Are Individuals Who Receive Acute Care Services In A Hospital Called?
Disquisitional Access Infirmary is a designation given to eligible rural hospitals by the Centers for Medicare & Medicaid Services (CMS). Congress created the Critical Access Infirmary (CAH) designation through the Counterbalanced Budget Human activity of 1997 (Public Law 105-33) in response to over 400 rural hospital closures during the 1980s and early 1990s. Since its creation, Congress has amended the CAH designation and related program requirements several times through boosted legislation.
The CAH designation is designed to reduce the financial vulnerability of rural hospitals and amend access to healthcare by keeping essential services in rural communities. To attain this goal, CAHs receive certain benefits, such as toll-based reimbursement for Medicare services. (run into What are the benefits of CAH status?)
Eligible hospitals must meet the following conditions to obtain CAH designation:
- Accept 25 or fewer acute care inpatient beds
- Exist located more 35 miles from another hospital (exceptions may apply – come across What are the location requirements for CAH condition?)
- Maintain an almanac average length of stay of 96 hours or less for acute intendance patients
- Provide 24/7 emergency care services
Congress as well created the Medicare Rural Hospital Flexibility Programme (Flex Program) in the Balanced Budget Act of 1997 to back up new and existing CAHs.
This guide provides resources concerning the following CAH-related areas:
- Payment/reimbursement and fiscal information
- Regulations and information regarding CAH status and the Flex Programme
- Central organizations in the field
- Funding opportunities
- Challenges to performance
Oftentimes Asked Questions
- What are the benefits of CAH status?
- How does Medicaid reimburse CAHs?
- Are all the benefits of CAH status available in every state?
- What types of facilities are eligible for CAH status?
- What are the location requirements for CAH status?
- How many CAHs are there and where are they located?
- What are the quality balls and quality improvement options for CAHs?
- What is the Medicare Rural Infirmary Flexibility Program and how is it related to the CAH program?
- Where tin can I find CAH comparative information?
- Tin a CAH ain another healthcare facility?
- Tin a CAH add an off-campus, provider-based dispensary that does non encounter the CAH distance requirements?
- What are the requirements for relocating an existing CAH under the Necessary Provider replacement rules?
- Is there a limit on the length of stay for patients at CAHs?
- How many beds are immune?
- What is a swing bed?
- What emergency services are CAHs required to provide? What are staffing requirements for emergency services?
- What kinds of agreements does a CAH demand to take with an acute care hospital?
- Where tin I find examples of CAH network agreements, tools, and other materials?
- How do staffing and other requirements differ for CAHs, compared to general astute care hospitals?
- Are CAHs eligible for the 340B plan?
- What sources of capital funding exist for CAHs?
- What is the CAH survey process?
- What legislation has affected the Critical Admission Hospital program?
- What are Rural Emergency Hospitals?
- Who can answer questions near CAH status or reimbursement problems?
What are the benefits of CAH status?
CAH status includes the following benefits:
- Cost-based reimbursement from Medicare. Equally of January 1, 2004, CAHs are eligible for commanded cost plus 1% reimbursement. Nonetheless, as of April 1, 2013, CAH reimbursement is subject to a 2% reduction due to sequestration. In some states, CAHs may also receive cost-based reimbursement from Medicaid.
- Flexible staffing and services, to the extent permitted under state licensure laws.
- Capital improvement costs included in allowable costs for determining Medicare reimbursement.
- Access to Flex Program educational resources, technical aid, and/or grants.
For more information nigh CAH reimbursement and payment benefits, run into the Medicare Learning Network: Critical Access Infirmary booklet from CMS, the Small Rural Hospital and Clinic Finance 101 transmission from the Technical Assistance and Services Centre (TASC), or Medicare Payment Basics: Disquisitional Access Hospitals Payment System from the Medicare Payment Advisory Commission (MedPAC).
Critical Access Hospital (CAH) status does not guarantee a better financial situation. Some hospitals will find the cost-based reimbursement advantageous, and some volition not. Each infirmary must perform its ain financial assay to determine if being a Prospective Payment Organisation (PPS) hospital or a CAH would result in a better fiscal render. For financially distressed hospitals, even if CAH status leads to increased reimbursement, it may not put the infirmary in the black. In fact, some hospitals take closed even after converting to CAH status. The Flex Monitoring Team releases an annual CAH Financial Indicators Report that can be helpful in agreement financial performance of CAHs.
CAH condition should be considered or maintained only if it is appropriate for the community need and hospital service area. In detail, consideration should be given to the bed limit for CAHs and potential service lines and whether they are sufficient to run across community need.
CAH status does not necessarily hateful fewer services are offered compared to other facilities. Services offered by a CAH should be aimed to meet the customs'south unique needs. Therefore, the number and type of services offered in one community may be different than in some other community. A CAH tin can utilize a Community Health Needs Cess (CHNA) to guide its review of current and time to come services needs.
For information about payment methods, eligibility criteria, and financial performance, see Medicare Payment for Rural or Geographically Isolated Hospitals and 2016-18 Profitability of Urban and Rural Hospitals past Medicare Payment Nomenclature, which compare the post-obit designations:
- Disquisitional Access Hospital (CAH)
- Sole Community Hospital (SCH)
- Medicare-Dependent Hospital (MDH)
- Rural Referral Center (RRC)
How does Medicaid reimburse CAHs?
Each state determines how it volition reimburse CAHs for services through Medicaid. Several states utilize some form of cost-based reimbursement for CAHs, while other states follow a prospective payment system (PPS). Additionally, variation may exist between inpatient and outpatient payment policies.
The Medicaid and CHIP Payment and Access Commission (MACPAC) compiled each country's Medicaid payment policies for inpatient and outpatient services.
- Land Medicaid Payment Policies for Outpatient Hospital Services (July 2016)
State-specific payment details for CAHs are listed in row 28. - State Medicaid Payment Policies for Inpatient Hospital Services (December 2018)
Country-specific payment details for CAHs are listed in row 17.
For additional information about your state's payment policies, consult your State Rural Hospital Flexibility Program Contact.
Are all the benefits of CAH status available in every state?
No. Some states license CAHs under the aforementioned licensure rules as other hospitals, and CAHs must comply with those licensure rules. If those rules are stricter than the CAH CoP, the CAH is unable to benefit from the more flexible Medicare Weather condition of Participation (CoP) for CAHs and the related cost savings. In addition, five states — Connecticut, Delaware, Maryland, New Bailiwick of jersey, and Rhode Isle — do non have any hospitals with CAH condition, and therefore do not participate in the Flex Program.
What types of facilities are eligible for CAH status?
Facilities applying to get Critical Access Hospitals must be currently participating in the Medicare program and have a current license equally an acute care hospital. Hospitals airtight later November 29, 1989, and hospitals that have downsized to health dispensary or health center condition may also qualify for CAH status if they meet all of the CAH Conditions of Participation.
What are the location requirements for CAH status?
Critical Access Hospitals must exist located in rural areas and must meet 1 of the post-obit criteria:
- Be more than than a 35-mile drive from another hospital, or
- Exist more a fifteen-mile drive from another hospital in an expanse with mountainous terrain or merely secondary roads.
CAHs designated by their land every bit a Necessary Provider prior to January 1, 2006, are exempt from these altitude requirements. Run across the Centers for Medicare & Medicaid Services' Clarification of Critical Access Hospital (CAH) Rural Status, Location and Distance Requirements and Critical Admission Hospital (CAH) Recertification Checklist for Evaluation of Compliance with the Location and Distance Requirements for definitions.
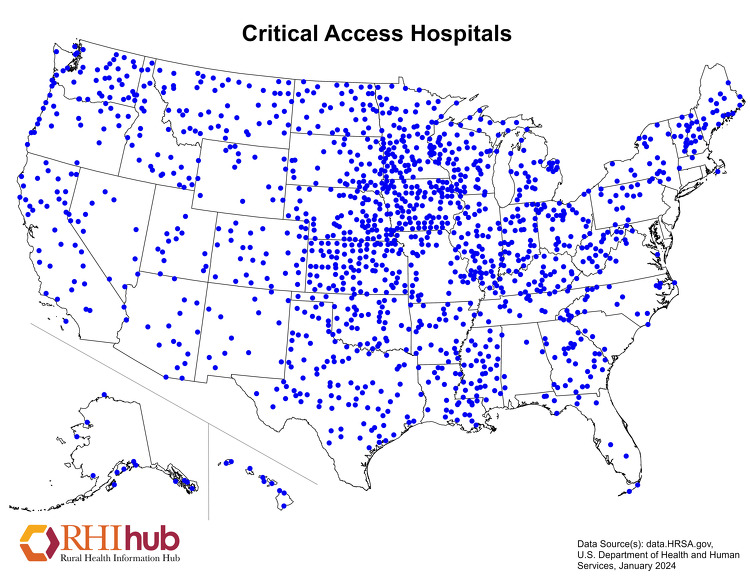
How many CAHs are there and where are they located?
The Flex Monitoring Squad maintains a list of Critical Access Hospitals, which includes the hospital name, metropolis, state, cypher code, and constructive date of CAH status.
As of July 16, 2021, there are 1,353 CAHs located throughout the United States.
The following map shows the locations of Disquisitional Access Hospitals across the United States. State-level healthcare facility maps are likewise available.
What are the quality assurance and quality improvement options for CAHs?
Critical Access Hospitals (CAHs) must have and maintain quality assurance arrangements with at to the lowest degree one of the following:
- One other CAH or infirmary that is part of the network
- Ane quality comeback organization (QIO) or equivalent entity
- Ane other appropriate and qualified entity every bit identified in the country'southward rural health care program, such as an accrediting body.
In improver to quality assurance, quality improvement is important to CAHs. The Medicare Beneficiary Quality Comeback Project (MBQIP), nether the Medicare Rural Hospital Flexibility (Flex) Program, aims to improve quality of care in CAHs by encouraging cocky-reported quality data, which are analyzed and used to inform activities at the facility. The Flex Monitoring Team's MBQIP Quality Measure Trends, 2011-2016 shows CAH operation trends and MBQIP reporting rates during that period. Co-ordinate to the May 2019 MBQIP Monthly, 99% of CAHs in the U.Southward. report on at least 1 domain and 93% reported quality measures in at to the lowest degree iii domains in 2018. Whatever CAH wanting to receive benefits or services from the state's Flex Program funding must participate in MBQIP and meet the minimum reporting requirements (or submit a waiver if necessary). The National Rural Health Resource Center also provides resources for State Flex Programs and providers regarding MBQIP, including Flex Eligibility Criteria for MBQIP Participation and Waiver Templates.
What is the Medicare Rural Infirmary Flexibility Program and how is it related to the CAH programme?
The Medicare Rural Infirmary Flexibility Plan (Flex Program) was created by the Balanced Budget Human activity of 1997 and is administered through the Federal Office of Rural Wellness Policy. The Flex Program encourages states to take a holistic approach to strengthening rural healthcare with a focus on Critical Admission Hospitals (CAHs) and their Rural Health Clinics, rural emergency medical services (Ems), and rural communities. The Flex Program provides federal cooperative agreements to eligible states to aid them reach their strategic goals, particularly in the following areas for Fiscal Years 2019-2023:
- CAH quality improvement (required)
- CAH operational and financial improvement (required)
- Population wellness improvement (optional)
- Rural emergency medical services (European monetary system) comeback (optional)
- Innovative model development (optional)
- Critical Access Hospital designation (required if requested)
Specific goals within each priority area are updated for each program bicycle to best reflect the needs of CAHs.
The Federal Office of Rural Health Policy likewise awarded supplemental funding to eight Country Flex Programs to conduct demonstration projects to build an bear witness base for rural Ems related to quality metrics and sustainable rural EMS models. Implementation of Flex European monetary system Supplemental Funding Projects: Year Ane Activities provides an overview of the implementation of the first year of these efforts, which spanned September 2019 to August 2020.
National infrastructure to back up the Flex Program includes:
- Federal Role of Rural Health Policy (FORHP) – Administers the Flex Program and its associated grants to states. Located within the Wellness Resources and Services Administration (HRSA).
- Technical Assistance and Services Center (TASC) – Provides information and technical assist to State Flex Programs and Disquisitional Access Hospitals. Located at the National Rural Health Resource Centre.
- Flex Monitoring Team – Conducts research and collects information on CAHs, evaluates the impact of the Flex Program, and maintains the listing of CAH locations across the country. As well operates and maintains the Disquisitional Access Hospital Measurement and Performance Assessment Organization (CAHMPAS).
- Rural Quality Improvement Technical Assistance (RQITA) – Seeks to better healthcare quality and health outcomes in rural communities by providing data and technical assistance to Land Flex Programs, Small Wellness Care Provider Quality Improvement grantees, CAHs, and other rural providers. Located at Stratis Health.
Where tin I notice CAH comparative data?
The Flex Monitoring Team has a number of resources that would allow you to benchmark your CAH or find data on CAH finances and quality measures. These include:
- The Disquisitional Admission Hospital Measurement and Performance Assessment Arrangement (CAHMPAS) – Offers the ability to compare data on community-benefit measures at a county and state level and quality indicators at a country level.
- CAH Financial Indicators Report: Summary of Indicator Medians by Country – Provides annual state-specific data on revenues, costs, average census, and more. The CAH Financial Indicators Primer and Calculator Resource explains how the measures are calculated and provides tools to enter your ain data.
- Patients' Experiences in CAHs: HCAHPS Results, 2018 – Provides country and national averages for CAH performance on the Infirmary Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey and state-specific reports.
- Hospital Compare Quality Measure Results for CAHs, 2018 – Offers state-specific CAH information on inpatient and outpatient quality-reporting measures from Hospital Compare.
- Critical Admission Hospital (CAH) State Profiles – Allows users to search for state-level reports on community benefit, quality, and financial indicators past twelvemonth.
- Community Bear upon and Do good Activities of Disquisitional Access, Other Rural, and Urban Hospitals, 2019 – Examines the economic and healthcare do good of Critical Access Hospitals (CAHs) on rural communities and enables State Flex Programs and CAH administrators to compare the community impact and benefit profiles of CAHs in their state to CAHs and other hospitals nationwide.
The National Rural Health Resource Centre'due south Population Health Toolkit incorporates County Health Rankings, Infirmary Compare, Medicare information, and Census data to help Disquisitional Access Hospitals (CAHs), Flex Coordinators, and rural wellness networks use a systems-based approach to move towards population health.
If you are interested in comparing the number of beds, operating rooms, or staff, apply the HRSA Data Explorer:
- Select "Health Care Facilities" and "Choose Indicators"
- Select indicators of interest, such equally "Facility Physicians Full-Time Equivalent," and "View Information"
- Nether "Facility Subcategory," type in "Critical Access" and select "Contains"
For additional quality reporting information, Medicare's Care Compare provides information on some CAHs. You lot can search by state, county, urban center, or zip code to compare up to three hospitals, or download CMS Provider Data Catalog datasets.
Can a CAH ain another healthcare facility?
According to Critical Access Hospital Measurement and Operation Assessment System (CAHMPAS) Data Summary, 60.iv% of Critical Access Hospitals managed Rural Wellness Clinics and 38.4% provided skilled nursing care in 2018.
A survey of Disquisitional Access Hospitals in Illinois institute CAHs are most likely to operate (versus own) dental offices, mental wellness practices, community health centers, retail pharmacies, and EMS, and were most interested in adding community wellness centers and behavioral health practices. The written report notes CAHs may choose to collaborate with or operate other facilities rather than owning them, nearly often citing financial or workforce concerns.
Regarding Federally Qualified Health Centers, meet Can another healthcare system, such as a Disquisitional Access Hospital, ain an FQHC? on the Federally Qualified Health Centers topic guide.
Fifty-fifty if a CAH does non own another healthcare facility, it can likewise benefit from collaboration and network agreements. Demonstrating Critical Access Hospital Value: A Guide to Potential Partnerships identifies potential partners for CAHs and discusses how CAHs can demonstrate their value to them. A Guide for Rural Health Care Collaboration and Coordination, a publication from the Health Resources and Services Administration (HRSA), describes how rural organizations and facilities, including CAHs, can develop partnerships to address the needs of their community. The National Rural Health Resource Center besides provides a number of examples of networks that included CAHs in its Network Spotlights.
See Who can reply questions virtually CAH status or reimbursement problems? for experts to contact for additional guidance on ownership problems.
Can a CAH add an off-campus, provider-based clinic that does not encounter the CAH distance requirements?
As of Jan i, 2008, all CAHs, including Necessary Provider CAHs that create or acquire an off-campus, provider-based facility, such as a dispensary or a psychiatric or rehabilitation distinct part unit of measurement, must meet the CAH distance requirement of a 35-mile drive to the nearest infirmary or CAH (or 15 miles in the instance of mountainous terrain or secondary roads). This provision excludes Rural Health Clinics, every bit defined under 405.2401(b), from the list of provider-based facilities that must comply with this requirement. Details most this requirement are bachelor in a final rule published in the Nov 27, 2007 upshot of the Federal Register as part of the Medicare Program: Changes to the Infirmary Outpatient Prospective Payment Organisation and CY 2008 Payment Rates. See Department XVIII. Changes Affecting Disquisitional Access Hospitals (CAHs) and Hospital Conditions of Participation (CoPs), beginning on page 66877.
What are the requirements for relocating an existing CAH under the Necessary Provider replacement rules?
Disquisitional Access Hospitals that were granted Necessary Provider designation prior to Jan one, 2006, and choose to rebuild in a new location that does not meet the current distance requirements, are treated in the aforementioned manner as if they were building a replacement facility at the original location. In order to maintain CAH status and the necessary provider designation, the new facility must satisfy the following requirements:
- Meet the same criteria that led to its original land designation
- Serve at least 75% of the same service area
- Offer at least 75% of the aforementioned services
- Utilize at least 75% of the same staff in its new location
See the September 7, 2007, letter from CMS to state survey bureau directors titled Critical Admission Hospitals (CAHs): Distance from Other Providers and Relocation of CAHs with a Necessary Provider Designation for more than detailed information.
Is there a limit on the length of stay for patients at CAHs?
Critical Access Hospitals must maintain an annual average length of stay of 96 hours or less for their acute care patients. The following are not included when calculating the 96-hour average:
- Fourth dimension spent in the CAH as an outpatient
- Fourth dimension spent in a CAH swing bed
- Fourth dimension spent in a CAH distinct part unit of measurement (DPU)
How many beds are allowed?
CAHs may have a maximum of 25 astute care inpatient beds. For CAHs with swing bed agreements, any of their beds can exist used for inpatient acute care or for swing bed services. Whatever hospital-blazon bed which is located in, or adjacent to, any location where the hospital bed could be used for inpatient care counts toward the 25-bed limit.
Certain beds do not count toward the 25-bed limit, including examination or procedure beds, stretchers, operating room tables, and beds in Medicare certified rehabilitation or psychiatric distinct function units. For a complete list of beds that do non count toward the 25 bed limit, please see Section C-0211, §485.620(a) Standard: Number of Beds: Interpretive Guidelines of the CMS State Operations Manual: Appendix West.
What is a swing bed?
A swing bed is a bed that can exist used for either acute care or mail service-acute care that is equivalent to skilled nursing facility (SNF) care. The Centers for Medicare & Medicaid Services approves CAHs, and other hospitals, to furnish swing beds, which gives the facility flexibility to meet unpredictable demands for acute care and SNF care.
The Rural Monitor article History of the Swing Bed: A Expect Through the Rural Rearview Mirror describes the evolution of the swing bed program to encounter the acute and post-acute care needs of rural residents. Swing beds offer an alternative to skilled nursing facilities. This selection may be useful in rural areas, which are less likely to have a stand-alone SNF. In add-on, populations in rural areas tend to exist older, and swing beds are well-adjusted for treating health problems typically seen in aging patients. The most commonly reported need was for crumbling patients who require rehabilitation following their hospital stay, according to Why Use Swing Beds? Conversations with Hospital Administrators and Staff. Furthermore, swing beds help stabilize healthcare facilities' census and may provide financial benefits. Swing bed services in CAHs are eligible for cost-based reimbursement, while swing bed services in non-CAH small rural hospitals are paid under the SNF prospective payment system.
For these reasons, swing bed post-acute intendance is common in rural healthcare facilities. According to Mail-Astute Skilled Nursing Care Availability in Rural Usa, 56% of all rural counties have at least one facility that provides post-astute skilled nursing care through a swing bed program.
For more details about the swing bed program, see the Medicare Learning Network: Swing Bed Services fact sheet and the Rural Monitor article Understanding the Rural Swing Bed: More than than Merely a Reimbursement Policy.
What emergency services are CAHs required to provide? What are staffing requirements for emergency services?
Emergency Department Services
CAHs must provide 24-hour emergency services.
Qualifying medical staff must be onsite or on-call and available onsite inside 30 minutes at all times. Onsite response times may be extended to 60 minutes if certain frontier or remote area criteria are met.
The staff onsite or on-call must meet state licensure requirements. CAH Status of Participation: Emergency Services specifies that coverage may be provided past a doctor of medicine (MD) or doctor of osteopathy (Exercise), a physician assistant, a nurse practitioner, or a clinical nurse specialist with experience and training in emergency intendance. Nether temporary, limited circumstances, coverage may exist provided by a registered nurse. In a June seven, 2013, memorandum, CMS clarified these requirements by stating that under CAH CoPs, an Physician or DO is not required to exist bachelor in improver to a non-physician practitioner. Additionally, this requirement may be met in whole or in part through the use of an MD or Exercise via telemedicine.
Every bit of October 1, 2007, CMS requires that any hospital, including a CAH, that does not accept a physician on site 24 hours per solar day, vii days per week, provide a observe to all patients upon access. The notice must accost how emergency services are provided when a physician is not onsite. For more information, delight see page 47413 of the August 22, 2007, Federal Annals find, Medicare Programme; Changes to the Hospital Inpatient Prospective Payment Systems and Fiscal Yr 2008 Rates; Final Rule.
Emergency Medical Services
Different emergency department services, CAHs are non required to provide emergency medical services.
Characteristics and Challenges of Rural Ambulance Agencies – A Cursory Review and Policy Considerations notes that dissimilar Disquisitional Admission Hospitals, ambulance services are typically not reimbursed at-toll. Equally a upshot, many CAHs are non inclined to maintain an ambulance service. According to Community Impact and Benefit Activities of CAHs, Other Rural, and Urban Hospitals, 2019, 21.8% of Critical Access Hospitals provided ambulance services in 2019. However, after accounting for the office of hospital health systems and joint ventures, 52.iv% of CAHs had access to ambulance services. In addition, 47% of CAHs were designated equally certified trauma centers.
The Borderland Community Wellness Integration Project (FCHIP) Demonstration, a joint demonstration projection between the Centers for Medicare & Medicaid Services and the Federal Part of Rural Health Policy, reimbursed 2 participating CAHs 101% of reasonable costs of furnishing Medicare Part B ambulance services instead of being paid under the Medicare ambulance fee schedule. These CAHs utilized the funding to provide increased stipends to volunteer emergency medical technicians (EMTs), concur additional EMT grooming classes, and purchase equipment. Although FCHIP initially ended in 2019, the Consolidated Appropriations Human activity, 2021, extended the program for an additional 5 years.
For more than information on Emergency Medical Services in rural communities, see RHIhub's Rural Emergency Medical Services (European monetary system) and Trauma topic guide.
What kinds of agreements does a CAH need to have with an astute care hospital?
As part of the agreements provision in the CAH Weather condition of Participation, a CAH must develop agreements with an acute intendance hospital related to patient referral and transfer, communication, and emergency and not-emergency patient transportation. The agreement must include at least one other infirmary that furnishes acute care services and can receive transfers of patients requiring services that are non available in the CAH.
The CAH may also have an understanding with its referral hospital for quality assurance, or choose to accept that agreement with some other system. Land networking requirements vary. For more information on quality balls options, run into What are the quality assurance and quality improvement options for CAHs?
Where can I observe examples of CAH network agreements, tools, and other materials?
RHIhub'due south Resource past Topic: Critical Access Hospitals lists hundreds of resources from organizations across the country. Yous can narrow the list past selecting resource blazon "Tool" for a number of financial and quality tools specific to CAHs.
The Arizona Critical Access Hospital Designation Manual provides samples of a:
- Rural Health Network Agreement (p. 23-27)
- Rural EMS Understanding (p. 28)
- Community Needs Assessment Template (p.31-33)
How practice staffing and other requirements for CAHs differ from those of full general acute care hospitals?
Under the Medicare Conditions of Participation (CoP), CAHs are granted greater staffing flexibility through 2 main provisions:
- Medical Staff
A Critical Access Infirmary must accept at least one MD or Practice physician, but that person is non required to be onsite. Advanced practice providers, such every bit physician assistants, nurse practitioners, and clinical nurse specialists can exist an independent office of the medical staff and can provide direct service to patients, including emergency services. - Nursing Staff
Full general astute care hospitals are required to have a registered nurse onsite 24/vii. Federal requirements allow for CAHs to close, and therefore have no nursing staff on duty, if the facility is without inpatients. Additional requirements vary by state. For instance, some states may offer flexibility by allowing an LPN to cover a shift in place of an RN when there are no acute patients. Contact your state survey agency for details.
CAHs must continue to meet their state licensure laws if those are stricter than the Medicare CoP.
Bated from staffing differences, requirements for CAHs and full general acute care hospitals are very similar. CAHs must encounter the requirements for the services they cull to provide. For example, if a CAH provides surgical services, it must meet the aforementioned relevant surgery requirements equally a general acute intendance infirmary.
Some issues may vary from state to state based on land licensure laws or other factors. To find out more than about your state's requirements, contact your State Rural Hospital Flexibility Plan Contact.
Are Critical Access Hospitals eligible for the 340B program?
The 340B programme allows certain eligible healthcare facilities to buy prescription and non-prescription medications at reduced cost. Critical Admission Hospitals that meet the eligibility criteria are able to participate in the 340B program as a Covered Entity. A 2018 report from the Government Accountability Part indicated that 77% of all CAHs participated in the 340B programme in 2016 and accounted for 45% of all hospitals participating in the program that yr.
See RHIhub's Rural Pharmacy and Prescription Drugs topic guide for more information virtually the 340B programme.
What sources of upper-case letter funding exist for CAHs?
Critical Access Hospitals (CAHs) qualify for a multifariousness of capital funding opportunities, such as grants and loans. Among others, the following 2 federal programs focus on helping CAHs with their capital funding needs:
- USDA Community Facilities Loan and Grant Plan – Provides funding to construct, expand, or improve rural healthcare facilities, including CAHs.
- HUD Section 242: Infirmary Mortgage Insurance Program – Helps rural healthcare facilities finance new construction, refinance debt, or purchase new equipment such as hospital beds and office machines.
Visit the funding department of this guide and the Capital Funding topic guide for additional opportunities and data.
What is the CAH survey process?
A facility interested in CAH status should contact its state survey agency to asking application materials. The state agency will review and forward the application to a CMS regional part. The CMS regional office will qualify a survey, and the state agency will then contact the facility to conform a survey engagement. The survey will verify that the CAH meets the federal facility requirements. Details about the survey procedure are available in Appendix W of the CMS State Operations Manual.
A facility will also demand to be recertified by the state survey bureau on a schedule consistent with the survey guidelines issued past CMS each year. A facility may be decertified if a state of affairs or issue presents immediate jeopardy and is not resolved quickly. Details about the recertification process are in Chapter 2 of the CMS Country Operations Manual.
Additionally, facilities may obtain deemed status if accredited past a CMS-approved Medicare accreditation organization. In the case of a deemed provider, the state bureau does not conduct an initial survey. While the facility seeking deemed status must yet contact the state agency to learn the Medicare and/or Medicaid certification materials, initial certification and subsequent recertification is performed by the accrediting system. CMS maintains a list of Approved Accreditation Organization Contacts for Prospective Clients. The post-obit accreditation organizations are approved for CAH certification:
- DNV GL – Healthcare (DNV GL)
- The Joint Committee (TJC)
What legislation has affected the Disquisitional Access Hospital programme?
Co-ordinate to the American Hospital Association, several pieces of legislation have modified the Critical Access Hospital (CAH) program since its creation through the Counterbalanced Budget Human action of 1997. The post-obit legislation are integral to the Critical Access Hospital (CAH) plan:
- Balanced Budget Human action (BBA) of 1997
Created the CAH programme, outlining all details of the programme including eligibility and operational regulations. - Medicare, Medicaid, and SCHIP Balanced Budget Refinement Act (BBRA) of 1999
Corrected unanticipated agin payment and regulatory consequences of the BBA of 1997. - Medicare, Medicaid, and SCHIP Benefits Comeback and Protection Act (BIPA) of 2000
Provided further exemptions and reimbursement improvements to CAHs, which strengthen the overall program. - Medicare Prescription Drug, Comeback, and Modernization Act (MMA) of 2003
Enhanced CAH payments, expanded bed-size flexibility, provided connected funding for the Medicare Rural Hospital Flexibility (Flex) Program grants, and increased Medicare payments to 101% of reasonable costs. It as well enacted a sunset of the necessary provider provision, effective January 1, 2006. - Medicare Improvements for Patients and Providers Act (MIPPA) of 2008
Further expanded Flex grants, and allowed CAHs to receive 101% of reasonable costs for clinical lab services provided to Medicare beneficiaries fifty-fifty if the specimen was collected offsite or at another CAH-operated facility. - American Recovery and Reinvestment Human activity (ARRA) of 2009
Created several grant, loan, and incentive programs to support the adoption of new health information technology (Striking) in CAHs. - Patient Protection and Affordable Care Act (ACA)
Included several efforts aimed at reducing workforce shortages, such equally expanding Area Health Educational activity Centers (AHECs) and further investing in the National Wellness Service Corps. It as well allowed CAHs to participate in the 340B program, making reduced cost pharmaceuticals attainable in rural communities. - Budget Control Deed of 2011
Imposed mandatory beyond-the-board reductions in federal spending to accomplish $1.two trillion in budget savings over a 10-twelvemonth period (also known as sequestration). - Bipartisan Budget Act of 2013/Pathway for SGR Reform Act of 2013
Extended sequestration for an additional two years (2022 and 2023) beyond the catamenia specified in the Budget Command Act of 2011 at the same percentage of spending. The Bipartisan Budget Acts of 2015 and 2018 extended sequestration through 2027. The Coronavirus Assistance, Relief, and Economic Security (CARES) Act further extended sequestration through financial year 2030. However, the CARES Act too paused sequestration amid the COVID-19 pandemic, and legislation passed in April 2021 extended the intermission through December 2021.
RHIhub's Rural Health Policy guide provides additional information on policies and legislation affecting rural healthcare.
What are Rural Emergency Hospitals?
The United states of america Congress established the Rural Emergency Hospital (REH) as a new Medicare provider blazon in the Consolidated Appropriations Act, 2021. Effective January 1, 2023, this police force will allow Critical Access Hospitals and other modest rural hospitals meeting eligibility criteria to convert to Rural Emergency Hospital (REH) status. REHs will be reimbursed at 105% of the outpatient prospective payment organisation (OPPS) for emergency and outpatient care services in improver to a fixed monthly payment. Different Critical Access Hospitals, REHs volition not be allowed to provide inpatient services.
Run across RHIhub's Rural Hospitals topic guide for additional data on Rural Emergency Hospitals.
Your State Rural Hospital Flexibility Program Contact can provide ongoing guidance near CAH issues. Other of import contacts include:
- CMS Regional Office Rural Wellness Coordinator – for questions about CMS regulations
- Land Survey Agency – for survey and certification questions
- National Rural Health Resource Center's Technical Help and Services Center (TASC) – for technical assistance, information, and other resources
- Medicare Administrative Contractor (MAC) – for questions about Medicare claims, reimbursement, and billing problems
What Are Individuals Who Receive Acute Care Services In A Hospital Called?,
Source: https://www.ruralhealthinfo.org/topics/critical-access-hospitals
Posted by: shoemakerwarl1992.blogspot.com


0 Response to "What Are Individuals Who Receive Acute Care Services In A Hospital Called?"
Post a Comment